Shingles: More Than Just a Rash
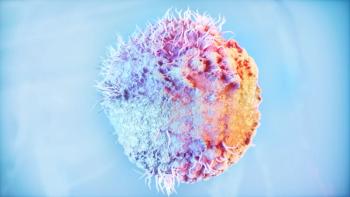
Herpes zoster can take a toll on the entire body.
Shingles (herpes zoster, or
When shingles occurs on the face, for example, early symptoms may include headache, general malaise, or fever. “When shingles involves branches of the trigeminal nerve, which innervates the region around the eye, eyelid swelling, conjunctivitis, ocular pain, light sensitivity, or visual changes may result,” explained Sarina B. Elmariah, MD, PhD, a board certified dermatologist at Massachusetts General Hospital.
Some forms of shingles are identified by their location on the body and have their own symptoms and complications. In cases of
Dr Elmariah said that early warning signs that a case of shingles may be more complicated than usual include taste or hearing changes, severe headaches, sensory loss, muscle weakness, and bladder or bowel dysfunction, which may signify encephalitis, meningitis, or myelitis. She advises her patients who experience shingles symptoms to seek care immediately from their health care provider and to start anti-viral therapy as soon as possible. She also encourages them to cover any blisters, erosions, or open skin to limit the spread of the virus.
“It is also important for individuals with shingles to distance themselves from immunocompromised individuals, pregnant women, or those who have not been vaccinated against chickenpox, as these populations can face serious complications if they were to become infected,” she said.
Finally, Dr Elmariah highly recommends the shingles vaccine Shingrix to her eligible patients, including immunocompetent individuals who are 50 and older and immunocompromised individuals under 50 years old. “Shingrix not only reduces the risk of experiencing the shingles rash, but it also limits the severity of disease and reduces the risk of postherpetic neuralgia even in those who do develop the rash,” she noted.
The
Reference
1. Shingrix Recommendations. CDC. Last reviewed January 25, 2018. Accessed October 30, 2020.
Newsletter
Pharmacy practice is always changing. Stay ahead of the curve with the Drug Topics newsletter and get the latest drug information, industry trends, and patient care tips.