Focus On Obesity Management Before Addressing Comorbidities
The latest guidelines advise managing obesity first, then treating a patient’s other conditions to produce optimal outcomes.
In 2015, authors of an article published in the Journal of Clinical Endocrinology and Metabolism1 urged the treatment of weight problems in a patient first, followed by treatment of comorbidities such as hypertension, impaired glucose tolerance, and more. “It’s an entirely new approach to the treatment of the disease. The old paradigm was to treat each comorbidity with medications, then manage obesity, which caused the original problem in the first place. The new paradigm is to manage the obesity first, with lifestyle changes and medications, then manage the remainder of the comorbidities that have not responded,” said Caroline Apovian, MD, codirector of the Center for Weight Management and Wellness at Brigham and Women’s Hospital and professor of medicine at Harvard Medical School in Boston, Massachusetts.
Person stepping on scale / terovesalainen - stock.adobe.com

Today, she still stands by this approach. “Obesity is the No. 1 reversible cause of death in westernized countries,” she said. “It leads to earlier mortality; so, if it starts young, these newer generations will not live as long as current generations. Obesity causes type 2 [diabetes (T2D), coronary artery disease, congestive heart failure], arthritis, and cancers. [T2D] is the most dangerous, and it can be almost eradicated in humans with weight control early on.”
Because weight gain has long been associated with an increased risk of these and other conditions, approvals over the past several years of semaglutide (Wegovy), tirzepatide (Zepbound), and liraglutide (Saxenda), have become well-known treatments for weight loss. Part of the family of medications known as glucagon-like peptide-1 agonists, they mimic a hormone released when food is eaten. Helping the body to create more insulin, they reduce the amount of sugar the liver makes, slow down the digestion process, and reduce appetite.2
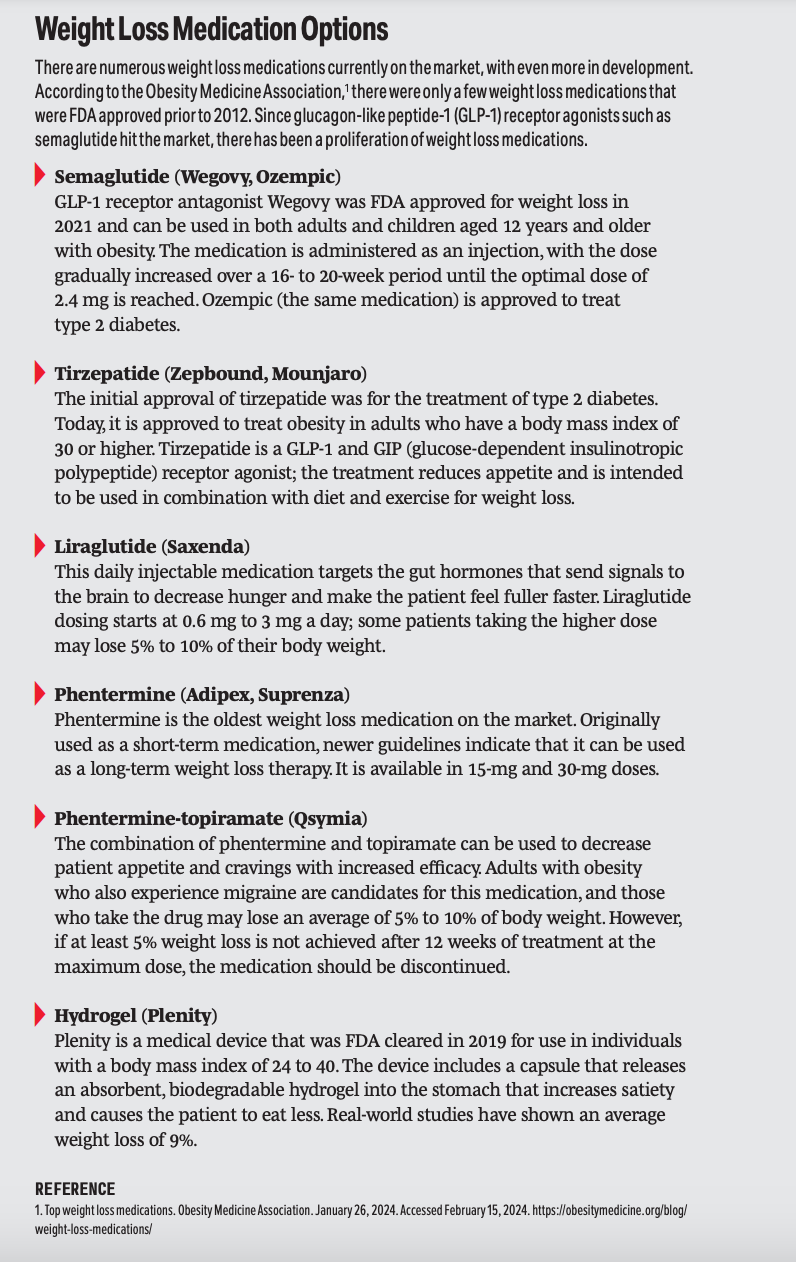
The concept of focusing on weight management first is a relatively new way of treating someone who is overweight or who has obesity coexisting with other conditions. In 2014, a report from the American College of Cardiology, the American Heart Association Task Force on Practice Guidelines, and The Obesity Society,3 which provided guidelines for the care of patients with cardiovascular risk, high cholesterol, and overweight and obesity, did not take into account weight loss medication. Although, arguably, in 2013, there were few FDA-approved options on the market (liraglutide was FDA approved for weight management in 2014).
Apovian, who was a coauthor of the 2013 guidelines, said these newer guidelines merely fill a gap that wasn’t addressed in 2013, and that the priority to manage weight and then attend to a patient’s comorbidities is important. “The prevalence [of obesity] is increasing. We need to control this disease,” she said.
Results of the SELECT trial (NCT03574597), which investigated whether semaglutide can reduce cardiovascular risk associated with overweight or obesity in the absence of diabetes, demonstrated that in patients with preexisting cardiovascular disease and overweight or obesity (but no diabetes), a weekly subcutaneous 2.4-mg dose of semaglutide was superior to the placebo in reducing the incidence of death from cardiovascular causes, nonfatal myocardial infarction, and nonfatal stroke at a mean follow-up of 39.8 months.4
READ MORE: FDA Approves Wegovy to Reduce Cardiovascular Risks in Overweight, Obesity
These new guidelines have been supported by other studies published in recent years. A 2017 study published in Current Obesity Reports stated that “one begins to see improvement in glycemic measures and triglycerides with small amount of weight loss, but with greater levels of weight loss, there is even greater improvement. In fact, the relationship between weight loss and glycemia is one that is very close. This is fortunate for diabetes prevention.”5
Danielle M. Alm, PharmD, BCPS, BCPPS, associate professor of clinical pharmacy at Philadelphia College of Pharmacy/Saint Joseph’s University in Pennsylvania, explained that pharmacists play a crucial role in patient education around these weight loss medications. “[Pharmacists] should provide comprehensive information about the mechanism of action, dosing instructions, potential [adverse] effects, and expected outcomes of the medication. Additionally, pharmacists can offer guidance on lifestyle modifications, such as diet and exercise, to complement the medication therapy,” Alm said.
“Furthermore, pharmacists should address barriers to adherence and persistence with weight loss medications. This may include addressing concerns about [adverse] effects, offering strategies to manage medication schedules, and providing support for behavior change. Pharmacists should collaborate with other health care providers, including physicians, dietitians, and psychologists, to ensure comprehensive care for patients using weight loss medications.”
READ MORE: Diabetes Resource Center
References
1. Apovian CM, Aronne LJ, Bessesen DH, et al. Pharmacological management of obesity: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab.2015;100(2):342-362. doi:10.1210/jc.2014-3415
2. GLP-1 agonists. Cleveland Clinic. Accessed January 30, 2024. https://my.clevelandclinic.org/health/treatments/13901-glp-1-agonists
3. Jensen MD, Ryan DH, Apovian CM. 2013 AHA/ACC/TOSguideline for the management of overweight and obesity in adults: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and The Obesity Society.Circulation.2013;129(25 suppl 2):S102-S138. doi:10.1161/01.cir.0000437739.71477.ee
4. Lincoff MA, Brown-Frandsen K, Colhoun HM, et al. Semaglutide and cardiovascular outcomes in obesity without diabetes. N Engl J Med. 2023;389(24):2221-2232. doi:10.1056/NEJMoa2307563
5. Ryan DH, Yockey SR. Weight loss and improvement in comorbidity: differences at 5%, 10%, 15%, and over. CurrObes Rep. 2017;6(2):187-194. doi:10.1007/s13679-017-0262-y
Q&A: Pharmacist-Led Diabetes Management Transforms Patient Care and Clinical Outcomes
June 28th 2025An ambulatory care pharmacist program in Washington State dramatically improved diabetes management by reducing A1c levels, increasing medication adherence, and providing comprehensive patient education.